Greater Trochanteric Bursitis, also known as Greater Trochanteric Pain Syndrome, is inflammation of the bursae near the greater trochanter, causing hip pain and discomfort. Exercise plays a key role in managing symptoms, improving mobility, and strengthening surrounding muscles. This guide provides a comprehensive overview of the condition, its causes, symptoms, diagnosis, and treatment options, with a focus on effective exercises and lifestyle modifications to alleviate pain and promote recovery.
1.1 Definition and Overview
Greater Trochanteric Bursitis, also known as Greater Trochanteric Pain Syndrome, is a condition characterized by inflammation of the bursae surrounding the greater trochanter, the bony prominence on the outer hip. This inflammation leads to pain, tenderness, and discomfort, often exacerbated by activities like sitting, lying on the side, or prolonged walking. The condition is commonly associated with overuse, repetitive hip movements, or direct trauma to the area. Exercise plays a central role in managing symptoms, with stretching and strengthening routines tailored to improve hip mobility and reduce discomfort. Early intervention and proper management are essential for effective recovery.
1.2 Importance of Exercise in Management
Exercise is a cornerstone in managing Greater Trochanteric Bursitis, as it strengthens the glutes and core muscles, improving hip stability and reducing pain. Stretching exercises enhance flexibility, while strengthening routines target the muscles around the hip joint, alleviating strain on the bursae. Low-impact aerobic exercises, such as swimming or cycling, promote mobility without aggravating the condition. Consistency in exercise routines is key to preventing recurrence and restoring functional movement. A well-structured exercise program, often guided by a physical therapist, is essential for long-term recovery and maintaining hip health.
Causes and Risk Factors
Greater Trochanteric Bursitis often results from repetitive hip movements, muscle imbalances, or direct trauma, with risk factors including prolonged sitting, arthritis, or prior hip surgery.
2.1 Anatomy of the Hip and Greater Trochanter
The hip joint is a ball-and-socket joint between the femur and pelvis, with the greater trochanter as a bony prominence on the femur’s upper end. This area is surrounded by muscles, tendons, and bursae, which reduce friction during movement. The greater trochanter specifically serves as an attachment point for gluteal muscles, playing a key role in hip stabilization and movement. The subgluteal and iliotrochanteric bursae near the trochanter can become inflamed, leading to pain and limited mobility. Understanding this anatomy is crucial for targeting exercises to strengthen surrounding muscles and improve joint function.
2.2 Common Causes of Greater Trochanteric Bursitis
Greater Trochanteric Bursitis often results from repetitive hip movements, overuse, or direct trauma, leading to bursae inflammation. Poor posture and biomechanics can cause uneven pressure on the hip joint, irritating the bursae. Obesity may exacerbate this by increasing hip pressure. Muscle imbalances or weakness in the glutes can lead to improper movement patterns. Age can make bursae less resilient. Tendon or ligament tears and inflammatory conditions like arthritis may also contribute. Addressing these factors through targeted exercises, posture improvement, and weight management can help prevent and manage the condition.
2.3 Risk Factors for Developing the Condition
Risk factors for Greater Trochanteric Bursitis include age, gender (more common in women), and obesity, which increases hip joint pressure. Repetitive activities like running or cycling can also contribute. Weak or tight hip muscles, poor posture, and previous hip injuries or surgeries elevate risk. Additionally, conditions like arthritis or diabetes may predispose individuals. Addressing these factors through targeted exercises, weight management, and ergonomic adjustments can reduce the likelihood of developing the condition and improve overall hip health.

Symptoms of Greater Trochanteric Bursitis
Common symptoms include hip pain, tenderness, and swelling near the greater trochanter, worsening with activity, prolonged sitting, or direct pressure on the affected area.
3.1 Common Symptoms and Pain Patterns
Greater Trochanteric Bursitis often presents with pain on the outer hip, tenderness over the greater trochanter, and swelling in the affected area. Pain typically worsens with activities like walking, climbing stairs, or prolonged sitting. Patients may experience discomfort when lying on the affected side or direct pressure on the hip. The pain can radiate down the thigh but usually does not extend below the knee. Symptoms may develop gradually, starting with mild discomfort and progressing to more persistent pain if left untreated. Early recognition of these patterns is key for effective management.
3.2 How Symptoms Progress Over Time
Symptoms of Greater Trochanteric Bursitis often begin with mild pain or discomfort on the outer hip, which may worsen over time. Initially, pain may occur only during specific activities like walking, climbing stairs, or prolonged sitting. Without treatment, the pain can become more persistent and may interfere with daily activities. Over time, the hip may feel stiff, and mobility can decrease. If left untreated, chronic inflammation and scar tissue formation can develop, leading to prolonged recovery. Early intervention is crucial to prevent progression and reduce the risk of chronic pain.
3.3 Distinguishing it from Other Hip Conditions
Greater Trochanteric Bursitis is often confused with other hip conditions due to overlapping symptoms. Unlike hip osteoarthritis, which typically causes groin pain, this condition causes pain on the outer hip and thigh. It can also be mistaken for hip labral tears or tendinitis, but the pain location and characteristics differ. Additionally, sciatica may present similarly, but it often involves radiating pain down the leg. Accurate diagnosis requires careful evaluation of pain patterns, physical examination, and imaging to rule out other hip-related conditions, ensuring appropriate treatment tailored to the specific cause of pain.

Diagnosis and Assessment
Diagnosis involves a thorough medical history, physical examination, and imaging tests like X-rays or MRIs to confirm Greater Trochanteric Bursitis and rule out other hip conditions.
4.1 Medical History and Physical Examination
A thorough medical history and physical examination are essential for diagnosing Greater Trochanteric Bursitis. The healthcare provider will assess symptoms, such as pain location, duration, and triggers, and evaluate tenderness around the greater trochanter. They may also check for pain during specific movements, like walking or climbing stairs. A physical exam will include palpation of the affected area and tests to assess hip mobility and strength. This process helps identify inflammation or irritation of the bursae and rule out other hip conditions, guiding an accurate diagnosis and appropriate treatment plan.
4.2 Imaging Tests for Confirmation
Imaging tests are crucial for confirming Greater Trochanteric Bursitis and ruling out other conditions. X-rays can identify bone spurs or fractures, while MRI provides detailed images of soft tissues, revealing bursae inflammation or tendon damage. Ultrasound is another effective tool, offering real-time visuals of the bursae and guiding corticosteroid injections if needed. These tests help confirm the diagnosis and assess the severity of inflammation, ensuring an accurate treatment plan tailored to the patient’s condition.
4.3 Differential Diagnosis Considerations
Differential diagnosis for Greater Trochanteric Bursitis involves distinguishing it from other hip conditions, such as osteoarthritis, tendinitis, or hip fractures. Pain patterns and physical exam findings, like tenderness over the greater trochanter, help differentiate it from conditions like sciatica or piriformis syndrome. Imaging tests, such as MRI or ultrasound, confirm bursitis by showing inflammation of the bursae. Lab tests may rule out inflammatory arthritis or infection. Accurate diagnosis ensures appropriate treatment, avoiding delays in addressing the root cause of hip pain.

Treatment Options for Greater Trochanteric Bursitis
Treatment involves a multidisciplinary approach, including rest, physical therapy, anti-inflammatory medications, and in severe cases, corticosteroid injections or surgery to address persistent symptoms and restore function.
5.1 Conservative Management Strategies
Conservative management focuses on reducing inflammation and alleviating pain through non-invasive methods. This includes rest, ice therapy, and anti-inflammatory medications. Physical therapy plays a central role, incorporating stretching and strengthening exercises tailored to improve hip mobility and strength. Additionally, lifestyle modifications such as weight management and ergonomic adjustments can help reduce strain on the hip joint. These strategies aim to restore function and comfort without surgical intervention, making them the first line of treatment for most patients.
5.2 Role of Physical Therapy in Treatment
Physical therapy is a cornerstone in managing Greater Trochanteric Bursitis, focusing on pain reduction, improved mobility, and strengthened muscles. Therapists design personalized exercise plans, including stretching and strengthening routines, to target the hip and surrounding tissues. Techniques like manual therapy and gait training can enhance joint mechanics and alleviate discomfort. Regular physical therapy sessions not only address current symptoms but also help prevent future flare-ups, promoting long-term recovery and functional independence.
5.3 When Surgery is Considered
Surgery is typically reserved for severe cases of Greater Trochanteric Bursitis where conservative treatments fail. Procedures may include bursectomy, where inflamed bursae are removed, or iliotibial band release to reduce tension. Surgery is considered when chronic pain persists, significantly impacting daily activities and quality of life. Patients are carefully evaluated, and surgery is recommended only after exhausting non-invasive options. Post-operative rehabilitation is essential to restore hip function and prevent recurrence, often involving guided physical therapy to ensure a smooth recovery process.
Exercise Program for Greater Trochanteric Bursitis
An effective exercise program for Greater Trochanteric Bursitis includes stretching, strengthening, and low-impact aerobic exercises to reduce inflammation, improve hip mobility, and strengthen surrounding muscles. A structured approach ensures gradual progression, minimizing discomfort while promoting recovery.
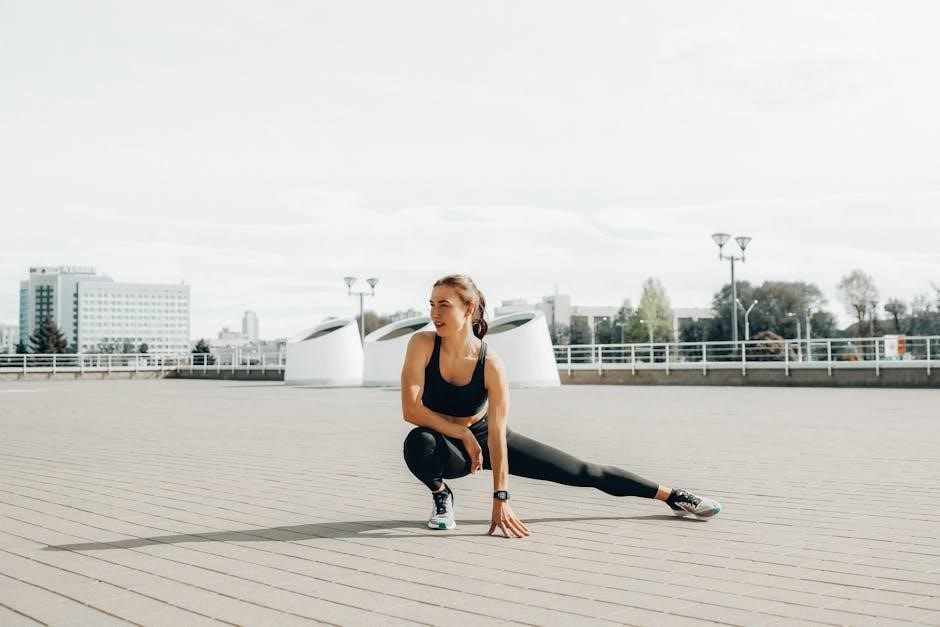
6.1 Stretching Exercises for the Hip
Stretching exercises are essential for reducing tightness and inflammation in the hip region. The piriformis stretch targets the piriformis muscle, which often contributes to trochanteric bursitis symptoms. The iliotibial band stretch helps alleviate tension along the outer thigh, while the hip flexor stretch improves flexibility in the front of the hip; These exercises should be performed gently to avoid aggravating the bursae. Holding each stretch for 20-30 seconds and repeating 2-3 times daily can promote relaxation of tight muscles and enhance joint mobility, making daily activities more comfortable. Regular stretching also supports long-term recovery by reducing muscle imbalances.
6.2 Strengthening Exercises for the Glutes and Core
Strengthening the glutes and core is vital for managing Greater Trochanteric Bursitis, as weak muscles can contribute to poor hip mechanics. Exercises like side-lying leg lifts target the gluteus medius, while clamshell exercises strengthen the gluteus maximus and hip stabilizers. Bird dogs and bridging exercises improve core stability and pelvic alignment. These exercises help reduce strain on the bursae by enhancing hip and pelvic stability. Performing 2-3 sets of 12-15 repetitions daily can improve muscle strength and endurance, reducing pain and improving functional mobility over time. Progressing exercises gradually ensures continued muscle development without overexertion.
6.3 Low-Impact Aerobic Exercises for Mobility
Low-impact aerobic exercises are essential for maintaining mobility in Greater Trochanteric Bursitis without aggravating the condition. Swimming and water-based exercises are ideal, as they minimize stress on the hips while improving cardiovascular health. Cycling on a stationary bike or using an elliptical trainer with low resistance is also beneficial, promoting blood flow and joint mobility. Gentle yoga and tai chi can enhance flexibility and balance. These activities should be performed at a moderate intensity for 20-30 minutes, 3-4 times weekly, to support recovery and maintain functional mobility without exacerbating inflammation or pain.
6.4 Progression of Exercises Over Time
Exercise progression for Greater Trochanteric Bursitis begins with gentle stretches and strengthening to avoid irritation. Initially, focus on low-intensity movements like hip flexor stretches and clamshell exercises. Gradually increase resistance using bands or light weights as pain subsides. Introduce single-leg stands and balance work to improve stability. Over time, incorporate dynamic movements such as side-lying leg lifts and controlled step-ups. Each progression should emphasize proper form to prevent recurrence. The goal is to enhance strength, flexibility, and functional mobility progressively, ensuring long-term recovery and reducing the risk of future flare-ups.

Specific Exercises for Pain Relief
Targeted exercises like side-lying leg lifts, clamshell exercises, and piriformis stretches help reduce inflammation and strengthen hip muscles, providing relief from Greater Trochanteric Bursitis pain effectively.
7.1 Side-Lying Leg Lifts
Side-lying leg lifts are effective for strengthening the hip abductor muscles, particularly the gluteus medius, which supports the pelvis and improves hip stability. To perform, lie on one side with legs straight, lift the top leg 12-18 inches, hold for 2-3 seconds, then lower slowly. Aim for 3 sets of 10-15 repetitions on each side. This exercise helps reduce pain and enhances functional movement, making it a cornerstone in Greater Trochanteric Bursitis management.
7.2 Clamshell Exercise
The clamshell exercise targets the gluteus medius muscle, essential for hip stability and reducing Greater Trochanteric Bursitis pain. Lie on your side with knees bent and feet touching. Slowly lift the top knee toward the ceiling without moving the feet, squeezing the glutes at the top. Hold for 2-3 seconds, then lower. Perform 3 sets of 10-15 repetitions on each side. This exercise strengthens the hip abductors, improving pelvic alignment and reducing lateral hip pain, making it a valuable addition to a rehabilitation program.
7.3 Piriformis Stretch
The piriformis stretch is effective for relieving tightness in the piriformis muscle, which can contribute to Greater Trochanteric Bursitis. Sit on the floor with the affected leg crossed over the thigh. Place your hand on the knee of the crossed leg and gently pull it toward your opposite shoulder. You should feel a stretch in the buttock area. Hold for 20-30 seconds and repeat 2-3 times on each side. Regular stretching can reduce muscle tension and alleviate hip pain, promoting better mobility and comfort.
7.4 Hip Abduction Exercises
Hip abduction exercises target the gluteus medius muscle, which is essential for hip stability and proper gait mechanics. Lie on your side with legs straight, then lift the top leg away from the bottom leg without bending the knee. Hold for 2-3 seconds, then slowly lower. Perform 3 sets of 10-15 repetitions on each side. Standing variations, using resistance bands or weights, can also be effective. These exercises strengthen the hip abductors, improving joint alignment and reducing pressure on the trochanteric bursae, thereby minimizing pain and inflammation over time.
Lifestyle Modifications for Managing Symptoms
Lifestyle changes, such as weight management, ergonomic adjustments, and activity modification, play a crucial role in alleviating Greater Trochanteric Bursitis symptoms and preventing recurrence.
8.1 Weight Management and Its Impact
Maintaining a healthy weight reduces pressure on the hip joint, minimizing strain on the bursae. Excess weight exacerbates inflammation, so weight management through diet and exercise can significantly alleviate symptoms. It helps prevent further irritation and supports overall joint health. Even moderate weight loss can reduce discomfort and improve mobility, making it easier to perform exercises and daily activities. Incorporating a balanced diet and regular physical activity is essential for managing Greater Trochanteric Bursitis effectively and promoting long-term recovery.
8.2 Ergonomic Adjustments at Work and Home
Ergonomic adjustments play a crucial role in managing Greater Trochanteric Bursitis by reducing strain on the hip. Ensuring proper chair height, workstation setup, and avoiding prolonged sitting can prevent irritation. At home, using supportive furniture and maintaining good posture during activities helps alleviate discomfort. Modify repetitive tasks to avoid awkward positions, and consider using cushions or pillows for better alignment. These adjustments create a more comfortable environment, reducing bursitis flare-ups and supporting recovery. Small changes can make a significant difference in managing symptoms and improving overall well-being.
8.3 Activity Modification to Avoid Aggravation
Modifying activities is essential to prevent aggravating Greater Trochanteric Bursitis. Avoid repetitive hip movements, heavy lifting, or prolonged sitting, which can irritate the bursae. Replace high-impact activities like running with low-impact options such as swimming or cycling. When performing unavoidable tasks, ensure proper body mechanics and posture to reduce strain on the hip. Taking regular breaks to stretch and move can also help minimize discomfort. By adjusting daily activities and avoiding overuse, individuals can effectively manage symptoms and support their recovery process.

Role of Physical Therapy in Recovery
Physical therapy is crucial for recovery, offering personalized exercise plans, manual therapy, and gait training to restore mobility, reduce pain, and strengthen hip muscles effectively.
9.1 Customized Exercise Plans by a Physical Therapist
A physical therapist creates tailored exercise plans to address individual needs, focusing on strengthening, stretching, and improving hip function. These plans often include exercises like side-lying leg lifts, clamshell exercises, and piriformis stretches to target specific muscle groups. The therapist assesses the patient’s condition and progresses the exercises gradually to enhance strength and mobility. Education on proper posture and movement techniques is also provided to prevent aggravation. Regular follow-ups ensure adjustments are made to optimize recovery and reduce pain, promoting long-term hip health and functionality.
9.2 Manual Therapy Techniques for Pain Relief
Manual therapy techniques, such as soft tissue massage, joint mobilization, and trigger point therapy, are effective for reducing pain and inflammation in Greater Trochanteric Bursitis. These hands-on methods target tight muscles and restricted joints, improving mobility and reducing pressure on the bursae. Techniques like deep tissue massage can break down adhesions in the IT band and glutes, while gentle joint mobilizations enhance hip movement. A physical therapist may also use myofascial release to relieve tension in connective tissues, further alleviating discomfort and enhancing the effectiveness of exercise programs.
9.3 Gait Training and Biomechanical Corrections
Gait training and biomechanical corrections are essential for addressing movement patterns that contribute to Greater Trochanteric Bursitis. A physical therapist can identify and correct abnormal gait mechanics, such as overstriding or limping, which may exacerbate hip pain. Techniques include posture re-education, foot strike modification, and core stabilization exercises to improve alignment and reduce stress on the trochanteric area. Biomechanical adjustments, like using orthotics or modifying walking surfaces, can further alleviate strain. These interventions aim to restore normal movement patterns, preventing recurrence and enhancing long-term mobility and comfort.

Recovery and Rehabilitation Timeline
Recovery from Greater Trochanteric Bursitis typically spans 6-12 weeks, with phases including acute pain management, progressive strengthening, and long-term prevention strategies to ensure full mobility restoration.
10.1 Acute Phase Management
The acute phase of recovery focuses on reducing pain and inflammation. Initially, rest and ice therapy are recommended to alleviate symptoms. Gentle stretching exercises, such as hip flexor and piriformis stretches, can be introduced to maintain flexibility without aggravating the condition. Pain management may include NSAIDs or corticosteroid injections. It’s crucial to avoid activities that worsen symptoms, such as prolonged sitting or repetitive hip movements. A physical therapist can guide gentle isometric exercises to strengthen muscles without putting stress on the hip joint. This phase typically lasts 1-2 weeks, aiming to stabilize the hip and prepare for progressive rehabilitation.
10.2 Subacute Phase Progression
The subacute phase, lasting 2-4 weeks, focuses on gradually increasing strength and mobility. Gentle strengthening exercises, such as hip abduction and clamshell exercises, are introduced to target the glutes and core. Low-impact aerobic activities, like swimming or cycling, are encouraged to improve mobility without stressing the hip. Posture correction and proper movement techniques are emphasized to avoid aggravation. Physical therapy plays a key role in progressing exercises safely and addressing any remaining pain. The goal is to restore functional movement and prepare for long-term maintenance and prevention of recurrence. Consistency is crucial during this phase.
10.3 Long-Term Maintenance and Prevention
Long-term maintenance focuses on preventing recurrence through consistent exercise and lifestyle adjustments. Regular stretching and strengthening exercises, such as hip abductions and core stabilizations, help maintain muscle balance. Proper posture and movement techniques reduce strain on the hip. Weight management and ergonomic adjustments at home and work further minimize risk. Incorporating low-impact activities, like cycling or swimming, supports joint health without overloading the hip. Addressing underlying risk factors, such as biomechanical issues, is essential for sustained recovery. Ongoing physical therapy can provide personalized guidance to ensure long-term success and prevent future episodes of bursitis.
Preventing Recurrence of Greater Trochanteric Bursitis
Preventing recurrence involves regular exercise, proper posture, and avoiding repetitive hip strain. Strengthening glutes and core muscles, along with maintaining flexibility, reduces the risk of future episodes.
11.1 Regular Exercise Routine
A consistent exercise routine is essential for preventing Greater Trochanteric Bursitis recurrence. Focus on strengthening glutes, core, and hip stabilizers through exercises like hip abductions and clamshells. Incorporate low-impact aerobics, such as swimming or cycling, to maintain mobility without overloading the hip joint. Stretching routines, including piriformis and iliotibial band stretches, help reduce muscle tightness. A well-structured weekly program, tailored by a physical therapist, ensures proper progression and avoids muscle imbalances. Regular activity not only reduces recurrence risk but also enhances overall hip function and long-term joint health.
11.2 Proper Posture and Movement Techniques
Proper posture and movement techniques are vital for managing Greater Trochanteric Bursitis. Avoiding prolonged sitting, maintaining a neutral spine, and ensuring hips are at a 90-degree angle can reduce hip strain. When moving, focus on controlled, smooth motions to prevent sudden jerks or twists; Incorporating ergonomic adjustments, such as using a supportive chair or cushion, can alleviate pressure on the trochanter. Additionally, practicing good gait mechanics during walking and avoiding overstriding can minimize hip joint stress. Tailoring posture and movement techniques with guidance from a physical therapist helps prevent recurrence and promotes long-term hip health.
11.3 Addressing Underlying Risk Factors
Addressing underlying risk factors is crucial for preventing Greater Trochanteric Bursitis recurrence. Identify and manage factors like prolonged sitting, obesity, or overuse from repetitive activities. Weight management through a healthy diet and regular exercise can reduce pressure on the hips. Improving flexibility and strength, particularly in the glutes and core, helps stabilize the hip joint. Avoiding repetitive movements that strain the trochanter is essential. A physical therapist can tailor interventions to address specific risk factors, promoting long-term hip health and reducing the likelihood of bursitis returning. Combining lifestyle changes with targeted exercises ensures sustained benefits.
Greater Trochanteric Bursitis can be effectively managed with targeted exercises, lifestyle changes, and addressing risk factors. Consistency in these approaches ensures symptom relief and prevents recurrence.
12.1 Summary of Key Points
Greater Trochanteric Bursitis is a common condition causing hip pain, often managed with targeted exercises, physical therapy, and lifestyle adjustments. Regular stretching and strengthening exercises, such as side-lying leg lifts and clamshell exercises, are essential for symptom relief and improving mobility. Weight management, ergonomic adjustments, and avoiding aggravating activities also play a crucial role. Early diagnosis through physical exams and imaging helps tailor treatment plans. Consistency in exercise routines and addressing underlying risk factors are key to preventing recurrence and achieving long-term recovery. Professional guidance ensures personalized and effective management strategies.
12.2 Importance of Consistency in Exercise and Lifestyle Changes
Consistency in exercise and lifestyle changes is vital for effectively managing Greater Trochanteric Bursitis. Regular performance of targeted exercises, such as side-lying leg lifts and clamshell exercises, helps strengthen the glutes and improve hip mobility. Adhering to a structured routine promotes long-term healing and prevents recurrence. Lifestyle adjustments, including weight management and proper posture, further enhance recovery. Over time, consistent efforts reduce inflammation, alleviate pain, and restore functional movement, making it easier to maintain an active and healthy lifestyle without discomfort or limitations.